Nutrition Management for Kidney Disease Patients
Fact Sheets:
|
Kidney Citizen: |
Relevant Articles:
|
E-Newsletter Articles:
|
>
Importance of Nutrition
A proper diet is essential for everyone, but especially important for patients suffering from chronic kidney disease (CKD) and end-stage renal disease (ESRD). Healthy kidneys help regulate the amount of water, minerals and electrolytes in the body. Your kidneys also work around the clock 24/7, 365 days a year. Those with diminished function need to adjust their diet to maintain the delicate balance. If you are on dialysis your diet needs to change even further, because the dialysis machine can’t replace the constant work your kidneys do.
A proper diet can help you manage your CKD and potentially prevent disease from progressing or developing in the first place. The Centers for Disease Control and Prevention’s data shows that more than 35% of people aged 20 or older with diabetes have CKD.(1) The leading risk factor for type 2 is being overweight.(2) So by combining a healthy diet with exercise, it is possible to reverse the current trend of increasing numbers of CKD patients in the United States.
Of course not every case is preventable, but eating better in general will help you live a higher quality life. Recent studies have even shown that diets low in protein can even delay development of ESRD (Low protein Diets for Chronic Kidney Disease in non-diabetic adults.(3)
This class will provide you with the tools and information to maintain or start a healthy diet and features information for pre-dialysis, dialysis and transplant patients. Regardless of your status, eating properly will give you more energy and help you live a longer life.
Please note that you should see your medical team before you start any major changes to your diet.
Kidney Friendly Diet
Choosing the right foods
Your diet will vary based off of your general needs, but will be most impacted by your stage of kidney failure and if end-stage renal disease, what type of dialysis treatment you are receiving.
An example from the recommended diet chart [9] is the amount of protein recommended for pre-dialysis and for dialysis patients.
Protein
Studies have shown that a low protein diets (hypoproteic) can help postpone dialysis. (1)
Protein is important in your diet because it helps keep the body nourished and healthy to fight off potential infections, repair tissue and for growth. Quality sources of protein include lean red meat, chicken, turkey, fish, lean pork, dairy and egg products. To keep a healthy diet overall it is best to select trimmed cuts of meat or low fat dairy. Nuts and beans are also a good source of protein, but also contain phosphorus.
The chart below was derived from data in the United States Department of Agriculture (USDA) National Nutrient Database for Standard Reference, Release 20.
|
Type of Protein Source |
Amount of Protein in Grams2 |
|
Poultry |
|
|
Chicken Breast (1/2 piece) |
26 |
|
Turkey (3oz) |
24 |
|
Ground Turkey (1patty) |
22 |
|
Beef |
|
|
Top Round (3oz) |
31 |
|
Veal (3oz) |
30 |
|
Ground Beef |
22 |
|
Pork |
|
|
Pork Chop (3oz) |
25 |
|
Pork Shoulder (3oz) |
27 |
|
Ham (3oz) |
18 |
|
Seafood |
|
|
Lobster (3oz) |
17 |
|
Crab (3oz) |
16 |
|
Shrimp (6large) |
10 |
|
Fish |
|
|
Fresh Tuna (3oz) |
25 |
|
Canned Tuna (3oz) |
21 |
|
Salmon |
23 |
|
Eggs |
|
|
Egg substitute (1/4 cup) |
7 |
|
Egg Cooked (1egg) |
6 |
|
Egg White (1egg) |
3 |
|
|
|
|
Beans and Nuts |
|
|
Kidney beans (1 cup) |
15 |
|
Lima beans (1 cup) |
15 |
|
Mixed nuts (3oz) |
15 |
Calcium
Calcium is another important element in a kidney friendly diet. Healthy kidneys help balance the amount of calcium and phosphorous in the body to promote bone growth and maintenance. Too much calcium can lead to harmful hardening of vessels and too little leads to weak bones. In many dialysis patients phosphorus levels will be higher and additional calcium might be needed to restore the balance. Calcium is found in most dairy products, but these also normally contain high levels of phosphorus. Calcium supplements are an option and sometimes calcium based phosphate binders are prescribed to increase calcium and lower phosphorous levels. If calcium levels are too high there are also options. Calcimimetics can be prescribed that mimic the action of calcium and lower the amount of calcium in your body.
Your dietician will also be able to point out foods that are high in calcium. (please note many items on this list contain high levels of phosphorus)
- Dairy such as Milk, Cheeses, Yogurt and ice cream
- Spinach
- Broccoli
- Rhubarb
- Tofu
- Oranges
- Flax seeds
- Quinoa
- Nuts
- Now many common foods have added calcium (calcium fortification or enrichment) including
- Breakfast cereals and bars
- Breads
- Juices
- Margarines
- Sports drinks
- Pancake or biscuit batter
- Crackers
- Soy or rice milk
- A few foods contain calcium and low phosphorous
- Two teaspoons of cinnamon has 50mg of calcium and no phosphorous
- Two teaspoons of basil have 63mg of calcium and only 15mg of phosphorous. (2)
Potassium
Potassium is also important in your diet because potassium levels control nerve and muscle functions. Since healthy kidneys remove excess potassium, most pre-dialysis and dialysis patients have too much potassium in their diet. Potassium intake is less of an issue for PD patients and more than three times weekly, hemodialysis patients, due to the more constant cycling of fluid.
Hyperkalemia or high levels of potassium in the body is associated with a significant increase in an irregular heartbeat and sudden death. (3)
It is difficult to limit potassium in your diet, since most foods have at least some in them.
A few helpful steps to keep your level lower includes:
- Watching portion sizes of fruits and vegetables
- Rinsing canned fruits and vegetables
- Replace dairy products with non-dairy substitutes
- Avoid salt substitutes
- Try leaching (a soaking process before cooking) your vegetables
- Track your potassium levels and share any drastic changes with your dietician
|
Category |
Eat this |
Not that |
|
Fruits |
Apple |
Bananas |
|
|
Plum |
Oranges |
|
|
Berry |
Raisins |
|
Vegetables |
Zucchini |
Acorn/Butternut Squash |
|
|
Bell pepper |
Tomato |
|
|
Green bean |
Spinach |
|
Dairy |
Nondairy creamer |
Milk |
|
|
Sherbet/popsicle |
Ice Cream |
|
|
Cream Cheese |
Cheese |
|
Snacks |
Pretzels |
Nuts or Seeds |
|
|
Lemon flavored deserts |
Chocolate flavored |
|
|
Sugar cookies |
Molasses cookies |
|
|
|
|
Sodium
Sodium is one your bodies’ major electrolytes that helps control the fluid content of your tissues and cells. Most people know sodium as salt, but salt is a compound made up of sodium and chloride. Healthy kidneys remove excess sodium from the body. Too much sodium is an issue because fluid will build up leading to higher blood pressure and potentially heart failure. Sodium will also make you feel thirstier and make it more difficult to keep within your recommended fluid restrictions. PD patients don’t need to watch their sodium intake as closely as HD patients, but still need to limit their sodium intake for their overall health. Many foods that you eat have sodium, and of course some are better than others.
High levels of sodium can lead to:
- Swelling (edema) throughout your body
- High blood pressure (hypertension)
- Heart failure
- Shortness of breath
Low sodium choices include:
- Fresh fruits and vegetables
- Unsalted popcorn
- Breads
- Pastas
- Unprocessed meats
High sodium choices to avoid include:
- Processed meats such as ham and luncheon meats
- Chips
- Canned soups and vegetables
- Tomato juice
- Sports drinks
- Many fast or convenience foods
You can help manage your intake by:
- Keeping a food journal to track your dietary sodium.
- Recording your weight daily to track swelling.
- Limiting processed foods.
- Choosing low sodium alternatives and not adding additional salt to meals.
- Reading food labels and looking for hidden sodium in items like drinks or in canned goods.
- Using natural flavor enhancers like spices and herbs as a substitute for salt.
What about dining out?
Restaurants don’t have to be off-limits. You can stick with a kidney-friendly diet and still enjoy your favorite places to eat. Work with your renal dietitian and learn to plan ahead. He or she will be able to give you suggestions based off of the type of food you are going for. Also if you know you are going for a specific type of food you can limit that type of food in your other meals that day. For example if you are going out for Mexican and really want salsa then you can try to limit your potassium in the other items that you eat.
Remember restaurant portions are often larger than those you eat at home. You can always ask for half to be boxed up in the beginning or share a meal with your table.
Don’t be afraid to ask your server for special requests, such as sauce on the side or no salt. The worst thing they can do is say no. Also, remember to bring your phosphate binders with you and take them as directed with your meal.
Don’t get caught up on what you can’t have, but use this as an opportunity to try something new and enjoy!
|
INSTEAD OF |
TRY |
|
Mexican |
|
|
tomato-based salsa |
chili pepper salsa |
|
avocado, mango, papaya, guava |
fajitas where you can control the condiments you add |
|
beans, Spanish rice |
plain rice |
|
Italian |
|
|
tomato and cream sauces |
pesto sauce |
|
olives and cheeses |
Breaded calamari |
|
pizza with pepperoni, sausage, olives, anchovies |
(white pizza)pizza with chicken and peppers |
|
cheese ravioli with tomato sauce |
Grilled fish, veal picatta, shrimp scampi |
|
Asian |
|
|
extra soy sauce, fish sauce and MSG (monosodium glutamate) |
ginger, hot pepper oil |
|
fried rice |
steamed rice |
|
meat, fish and/or poultry mixed with sauce |
grilled fish and chicken, tempura, sushi (no California rolls with avocado) or stir-fried vegetables with sauce on the side |
|
Southern |
|
|
dried beans or black eyed peas |
string beans or corn |
|
salted/cured meats, sausages, bacon, salt pork |
fried chicken with the skin removed |
|
cooked greens or spinach |
Okra |
|
Fast Food |
|
|
milkshake |
small ginger ale or lemon-lime soda |
|
French fries, baked potato |
Rice |
|
large, super- or king-sized hamburgers or cheeseburgers |
regular or junior-sized hamburgers |
How to read food labels
Food labels are a great tool. They can help you choose healthier, more kidney-friendly foods. However, before you go to the grocery store, talk with your renal dietitian. Since you need to watch certain nutrients such as potassium and phosphorous that were highlighted earlier in this course. Your renal dietitian can tell you how many milligrams (mg) or how much you should have each day. Once you know this, you’re ready to shop. (4)
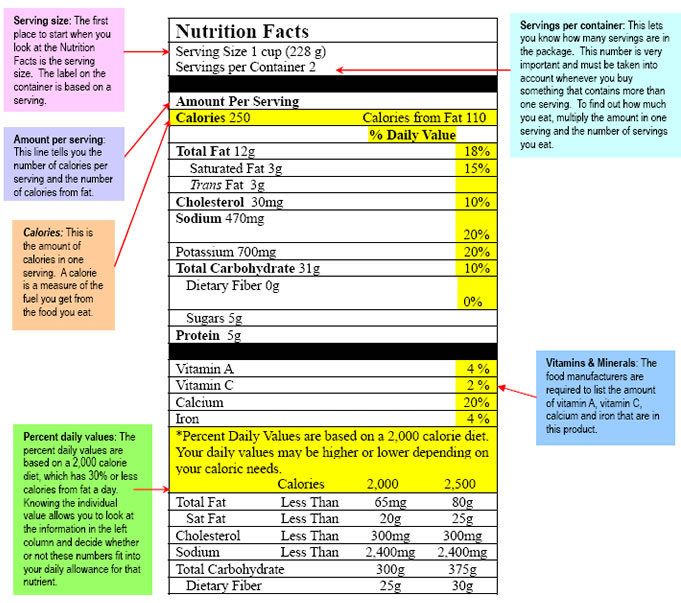
Food label tips:
- Items that you need to look out for are generally listed by content in grams or milligrams and percent daily values. It is important to remember that these values are for someone without kidney disease, so your needs may differ.
- A good rule of thumb is: food is low in phosphorus if it has fewer than 50 mg (or less than 5%). It’s high in phosphorus if it has more than 150 mg (or greater than 15%). (5)
- In general, a food is low in potassium if it has fewer than 100 mg (or less than 3%). More than 200 mg (or greater than 6%) is high. (6)
- Be aware. If a food label doesn’t list an item such as phosphorus in the example image, it doesn’t mean it isn’t in there.
- Another important thing to look at is serving size. For example a 20oz bottle of cola has 2.5 servings per bottle. If you drank the entire bottle, the values would need to be multiplied by 2.5.
- When in doubt, you can always save the labels and go over questions with your dietician.
Modify your favorite recipes
Cooking at home is a great way to save money and also put you in control of what you are eating. Living on a kidney friendly diet does mean that you have to limit or modify your recipes, but doesn’t mean you can’t enjoy meals with your family. In fact, sharing meals can be a good way to come together.
Keeping a journal and meal planning will help you stay on your diet and buying foods in bulk that can be used for multiple meals will keep your shopping costs down.
Family meals should be a source of comfort and not stress. Your family loves and cares for you so they will be willing to compromise. Getting everyone involved will help make those decisions easier.
There are many resources for dialysis friendly recipes here are some [10] compiled by DaVita that can be used as a starting point.
Also, your dietician and other members of your care team will be able to point you towards flavorful foods.
Just like dining out, this will give you a chance to try new items and expand your choices. Maybe you and your family will discover a new appreciation for pesto sauces instead of tomato based.
- Capusa C, Garneata L, Mircescu G, Stancu, S. Effects of a Supplemented Hypoproteic Diet in Chronic Kidney Disease. Journal of Renal Nutrition Volume 17, Issue 3 May 2007.
- USDA National Nutrient Database for Standard Reference, Release20. National Agriculture Library. http://www.nal.usda.gov/fnic/foodcomp/Data/SR20/nutrlist/sr20a203.pdf [11]
- Sudden Cardiac Death in Hemodialysis Patients: An In-Depth Review. American Journal of Kidney Disease. http://www.ajkd.org/article/S0272-6386(11)00595-6/fulltext#sec2.4 [12]
- Reading Nutritional Labels on Food Labels. Children’s Hospital of The King’s Daughters. http://www.chkd.org/HealthLibrary/Facts/Content.aspx?pageid=0416 [13]
- Phosphorus and your CKD Diet. National Kidney Foundation. www.kidney.org/atoz/content/phosphorus.cfm [14]
- Potassium and you CKD Diet. National Kidney Foundation. http://www.kidney.org/atoz/content/potassium.cfm [15]
Phosphorus: the where and why
Phosphorus is commonly found in foods such as dairy, organ meats, fish, poultry, eggs, whole grain products, nuts, and is unusually high in processed foods. Healthy kidneys help your body keep a balance of phosphorus and other minerals you need by filtering out what you don’t need.
When kidneys aren’t working well, phosphorus can build up, causing a condition known as hyperphosphatemia (hi-per-foss-fuh-TEE-mee-uh). If not treated, it can lead to serious health problems . (1) Your phosphorus level should be within the range of 3.5-5.5 mg/dL.2 Check with your dietitian or doctor if you don’t know your phosphorus level. A simple blood test will let you know what your levels are.
The chart below from the National Kidney Foundation Shows basic ways to substitute high phosphorous foods for low alternatives.
High phosphorus foods and alternatives
The chart below from the National Kidney Foundation Shows basic ways to substitute high phosphorous foods for low alternatives.
|
INSTEAD OF |
TRY |
||
|
FOOD |
Phosphorus |
FOOD |
Phosphorus (mg) |
|
8 oz milk |
230 |
8 oz nondairy creamer OR 4 oz milk |
100, 115 |
|
8 oz cream soup made with milk |
275 |
8 oz cream soup made with water |
90 |
|
1 oz hard cheese |
145 |
1 oz cream cheese |
30 |
|
1/2 cup ice cream |
80 |
1/2 cup sherbet OR 1 popsicle |
0 |
|
12 oz can cola |
55 |
12 oz can of ginger ale OR lemon soda |
3 |
|
1/2 cup lima or pinto beans |
100 |
1/2 cup mixed vegetables OR green beans |
35 |
|
1/2 cup custard OR pudding made with milk |
150 |
1/2 cup custard OR pudding made with nondairy creamer |
50 |
|
2 oz peanuts |
200 |
1 1/2 cup light salt low-fat popcorn |
35 |
Looking for hidden phosphorus
The following ingredients add phosphorous to foods:
- Sodium polyphosphate3
- Sodium tripolyphosphate
- Phosphoric acid
- Disodium phosphate
- Monosodium phosphate
- Potassium tripolyphosphate
- Sodium acid pyrophosphate
- Sodium hexametaphosphate
- Tetrasodium pyrophosphate
- Trisodium triphosphate
Certain buzz words such as “enhanced meat” found mainly in poultry products may contain hidden phosphorous. Another good rule of thumb is to avoid items that have additional fluid such as a brine added to them. In general brown colas contain high levels of phosphorous while clear drinks tend to have less. If you have a question and can’t tell by the label contents, ask your dietitian. Sometimes phosphorus is listed on labels as a more complex combination of ingredients. The following is a list of terms that means phosphorous is found in that food.
The effects of too much phosphorus
Symptoms of hyperphosphatemia may include cramps, numbness or tingling, itchy skin, bone pain, or joint pain. However, you may not experience any symptoms at all. It’s important that you work with your Renal Dietitian and monitor your blood levels regularly.
If high phosphorus levels are not treated, they can lead to:
- Sore, weak, and brittle bones
- Painful calcification (mineral buildup in your vessels and valves causing heart damage and failure.
- Recent studies show that increased phosphorus levels can cause calcium buildup in your vessels and valves causing heart damage and failure. (4)
Dialysis alone can’t get rid of the extra phosphorus. That’s why dietitians encourage patients to reduce the amount of phosphorus in their meals and sometimes prescribe medication like phosphate binders to help the body eliminate excess phosphorus.
Phosphate binders and how they work
Phosphate binders attach to the phosphorus in your food like a magnet to keep it from being absorbed by your body. The bound phosphorus can then be eliminated through the bowels. Some phosphate binders are chewable, while others are swallowed. It’s important to take your medication during your meals or immediately after eating. This lets the medicine bind to the phosphorus before food is absorbed by your digestive system, if too much time passes between when you eat and when you take your medication, the medication won’t work properly. You may not feel differently after taking your medication, but even if you cannot feel your binder working, you should still take your medication as directed. If you take your binder as prescribed, over time you should see an improvement of your phosphorus levels. Speak with your health care provider about what choice is best for you, how many pills to take each day, when to take them, and what to expect from treatment.
Phosphate Binder Options
Phosphate binders tend to fall within a few categories.
- Aluminum-based binders were the earliest binders that were used with the most common being aluminum hydroxide. Aluminum based binders though aren’t used much anymore, because of the toxic impact that aluminum has on the body. Examples of aluminum-based binders are Alu-Cap and Amphojel (aluminum hydroxide)
- Calcium-based binders are a group of binders that includes calcium acetate and calcium carbonate. They tend to not work as well as aluminum-based binders, but don’t have the toxicity issues of the early aluminum binders. Since these binders contain calcium, you will need to make sure you are not accidentally raising your calcium levels too much. Examples of calcium-based binders are PhosLo® (calcium acetate) and Tums (calcium carbonate).
- Aluminum and Calcium-free binders as the name implies don’t contain calcium or aluminum and are often made of sevelamer or seelamer carbonate. Examples of commonly prescribed aluminum and calcium-free phosphate binders are Fosrenol®, (lanthanum carbonate), Renagel® (sevelamer) and Renvela (sevelamer carbonate) (5)
Ask your physician if a binder is the right for you.
Ways to remember your medication
It is not unusual for people with kidney disease to forget their medication. When you are taking several kinds of medicine throughout the day, it can be tough to stay on top of all of them.
If you’re missing doses because you forget, try these tips:
- Use a watch with an alarm.
- Give your schedule to a caregiver or family member who can act as a double check.
- Set a notice on your email calendar or cell phone.
- Use a daily pill organizer box.
- Keep your medicine in a place where you can see it, but where children can’t reach.
- Use a calendar or daily planner to check off your medications as you take them each day.
- Work with someone on your health care team to create a chart you can post at home.
- List all your medications on it and check them off when you take them.
- Hruska K, Lund R, Matthew S, Pratt R, Qui P. Kidney International. July 2008: (74)2 148-157
- Phosphorus and your CKD Diet. National Kidney Foundation. www.kidney.org/atoz/content/phosphorus.cfm [14]
- Leon J, Sarathy-Sayre S, Sullivan C. Managing the Hidden Phosphorus in Foods: Beneficial Across all Stages of Kidney Disease. American Association of Kidney Patients. http://www.aakp.org/aakp-library/Hidden-Phosphorus/ [16]
- Kuhlmann, M. Management of hyperphosphatemia.Hemodialysis International 206; 10. 338-345.
- Clinical Practice Guidelines: Guideline 5 Use of Phosphate Binders in CKD. National Kidney Foundation. http://www.kidney.org/professionals/kdoqi/guidelines_bone/guide5.htm [17]
Safe or Scary? Navigating the Grocery Store : Education Webinar
What you should track as a dialysis patient
The two major types of dialysis therapy are hemodialysis (HD) and peritoneal dialysis (PD) and more information on both therapies can be found here [18]. There are several different varieties of HD and PD that vary based off of location (home and in-center), treatment times (day, night times) and the use of different machines, tubes and supplies. The most basic difference that will impact your diet is that HD is generally done less frequently than PD and uses a machine to filter your blood while PD uses your own abdomen as the filter. Since PD is done more frequently there isn’t as much time for there to be a buildup of waste products in the body. This means in general, there are less dietary and fluid restrictions for PD patients. However, the dialysate solution used in PD is sugar based and you will need to change your diet to deal with the extra sugar.
All dialysis patients need to watch the amount phosphorus (fos-fer-uhs), calcium (kal-see-um), potassium (poe-tass-ee-um), carbohydrates (kar-bo-hi-drates), sodium (so-dee-um) and fluids you take in.
- Phosphorus – is an essential mineral that plays a major role in bone development. Dialysis patients especially those on hemodialysis need to limit the amount of phosphorus they eat. Too much and it disrupts the body’s balance between phosphorus and calcium. This can lead to hardening of soft tissues and removes calcium from the bones making them weak.
- Calcium – is the most abundant mineral in the body and is needed for proper bone growth. Increased calcium is often important for dialysis patients to offset the additional phosphorus in their body.
- Potassium – is a mineral that is important for nerve and muscle function. Too much potassium may lead to muscle failure and in rare cases heart failure. Dialysis can only remove a fixed portion of potassium so it is important to limit foods that are high in the mineral. If you are a PD patient, you don’t have to limit potassium as much as other forms of dialysis.
- Carbohydrates – are in a class of nutrients that includes sugars and starches that provide a major source of energy in the body. Carbohydrates are important for all diets, but especially important for hemodialysis (HD) patients as they become a major portion of your diet. Peritoneal dialysis patients need to eat fewer carbohydrates because the dialysate solution is largely made of sugar and the body absorbs those calories.
- Sodium – is important because too much may increase blood pressure and lead to fluid retention. Sodium most commonly found in salt, can also lead to excess thirst. As a dialysis patient, when you go to treatment and there is excess fluid, the heart has to work harder to move the extra fluid leading to increased blood pressure and cramping. Sodium intake is most important for HD patients, because you are removing several days of excess fluid instead of more continually like PD and your natural kidney functions.
- Calories – a calorie is a unit of energy that is stored in the food we eat. The calorie listed on nutritional labels is knows as a kilocalorie or 1000 calories. However, for simplicity we will use the familiar term calorie instead of kilocalorie. It is important to get enough calories to fuel your daily activities. If you don’t have enough calories, you will break down your body’s protein. It will be important to work with your dietician to ensure you are getting the right amount of calories and from healthy sources.
The hard part of the renal diet is all of these nutrients and minerals are important for good health, but you have to keep them in balance and within recommended target levels. General guidelines for patients on dialysis, which will vary depending on body size, are listed below. Remember, these are just estimates.
Nutritional Guidelines for Chronic Kidney Disease Patients *In the example 150lb individual was the standard level. (5)
|
Nutritional Parameter |
Stages 1-4 CKD |
Stage 5 Hemodialysis |
Stage 5 Peritoneal Dialysis |
|
Calories (kcal/kg/d) |
35 < 60 yrs = 2380 Calories 30-35 ≥ 60 = 2040-2380 Calories |
35 < 60 yrs |
35 < 60 yrs |
|
Protein (g/kg/d) |
0.6-0.75 = 41-51 g |
1.2 = 81 |
1.2-1.3 = 81-88 |
|
Fat (% total kcal) |
For patients at risk for CVD, < 10% saturated fat, 250-300 mg cholesterol/d |
||
|
Sodium (mg/d) |
<1500 |
<1500 |
<1500 |
|
Potassium (mg/d) |
Match to lab values |
2000-3000 |
3000-4000 |
|
Calcium (mg/d) |
1200 |
≤ 2000 from diet and meds |
≤ 2000 from diet and meds |
|
Phosphorus (mg/d) |
Match to lab values |
800-1000 |
800-1000 |
|
Fluid (mL/d) |
Unrestricted w/ normal urine output |
1000 + urine 34 fl oz |
Monitor; 1500-2000 51-68 fl oz |
Please note that some foods have all nutrients such as phosphorus content listed on their nutrition labels, but most don’t. To find out where you can find this information, ask your renal dietitian.
Also each person is different and may require numbers that fall outside of the recommended guidelines.
- National Chronic Kidney Disease Fact Sheet 2010. Centers for Disease Control and Prevention. www.cdc.gov/diabetes/pubs/factsheets/kidney.htm [19].
- Prevention. American Diabetes Association. www.diabetes.org/advocate/our-priorties/prevention/?loc=DropDownADV-prevention [20].
- Fouque D, Laville M. Low Protein Diet for Chronic Kidney Disease in Non-diabetic Adults. The National Center for Biotechnology. www.hcbi.nlm.nih.gov/pubmed/19588328 [21]
- Sodium: Tips for People with Chronic Kidney Disease. National Kidney disease Education Program. www.nkdep.nih/gov/resources/nutrition-sodium-508.pdf [22]
- Beto J, Bansal V. Medical nutrition therapy in chronic kidney failure: integrating clinical practice guidelines. American Dietetic Association. 2004;104:404-409.
Fluid control
Monitoring that amount of fluid that you have between treatments is another important aspect of your diet.
Your fluid restriction is determined by several factors including urine output and weight gain between treatments. Fluid control is most important for hemodialysis patients because treatment is generally only done three times a week, compared to PD that is daily. Your dry weight is the amount of body weight minus the extra fluid that is stored in your body. It is similar to the weight after urination, in a person with fully functioning kidneys. As a dialysis patient, your dry weight is the amount that you weigh shortly after treatment. Using your weight change between treatments can help determine what your restriction will be.
Why should I care about restricting my fluids?
- Too much fluid between treatments can lead to cardiac arrest, heart disease, vein damage and blood pressure related issues. (1)
- Causes swelling
- Fluid can collect in your lungs
- Cramping during treatment
- Pulling too much fluid during treatment causes nausea and dizziness and drops in your blood pressure (1)
How do I control my fluid intake?
Your medical team will help you determine what your restriction will be, but it is up to you to manage your intake daily. Keeping a journal will help you track the amount you have each day.
Tips to control fluid:
- Minimizing your sodium is very important. As discussed here [23] sodium causes you to retain fluid and can make you feel thirstier.
- Evenly distributing your fluid throughout the day helps keep you from having dry mouth.
- Gum and tart items such as lemon juice can stimulate your salivary glands to wet your mouth.
- Small cups can help you portion out your liquid better.
- Ice does of course contain water, but can satisfy your thirst and not add a lot of fluid.
- Taking your medication with food like applesauce instead of water can save fluid.
- Understanding that almost everything you eat has water content and contains “hidden fluid”.
Hidden fluid
When most people think about fluid, they only think about liquids like water or juice. Drinks do have the most fluid content, but items such as yogurt, Jell-O and many fruits and vegetables have large hidden water content. Even items such as meat and bread have some moisture.
Although it is important to understand almost all items contain water, this information should just be another tool in your diet. You shouldn’t avoid corn because it has two ounces of water per ear, but should just understand that if you ate a several ears, you are adding fluid to your diet. Items to watch more carefully are those that are liquid at room temperature (things that melt) and high water fruits and vegetables.
Watching for hidden fluid can help you keep your weight gained between sessions down and make the process more enjoyable. If you need to take off less fluid during dialysis, you can have quicker treatments or have the filtration rate at a more comfortable level.
Ice cubes can be a great low fluid way to get rid of dry mouth, but remembers that ice is another common item that doesn’t get counted as fluid. A medium ice cube has approximately one ounce of water.
The following is a chart of some commonly eaten foods and their water content:
|
Food |
Amount of Fluid in Ounces |
|
Raisins (1 cup) |
1 |
|
1 Medium ice cube |
1 |
|
5 Prunes |
1 |
|
1 Ear of corn |
2 |
|
Lettuce (1 cup) |
2 |
|
Meats and poultry (3oz) |
2 |
|
Raw broccoli (1 cup) |
3 |
|
1 Medium peach |
3 |
|
Cranberries (1 cup) |
3 |
|
1 Bell pepper |
4 |
|
Ice cream (1 cup) |
4 |
|
1 Medium apple |
4 |
|
Strawberries (1 cup) |
5 |
|
Boiled peas (1 cup) |
5 |
|
1 Pear |
5 |
|
Carrots (2 cups) |
6 |
|
Boiled cauliflower (1 cup) |
6 |
|
1 Mango |
6 |
|
Yogurt (1 cup) |
7 |
|
Fruit cocktail (1 cup) |
7 |
|
Winter squash (1 cup) |
7 |
|
Jell-O (1 cup) |
8 |
|
Applesauce (1 cup) |
8 |
|
1 Papaya |
9 |
|
1 Wedge watermelon |
9 |
|
1 Medium cucumber |
10 |
- Glickman J. Stunning Consequences of Thrice-Weekly in Center Dialysis. Medscape Today. www.medscape.com/viewarticle/762480?src=mp&spon=38 [24]
Following a diet for diabetes and kidney disease
Both of these illnesses can be difficult to manage alone, but can create even more stress when you have to manage both. Many Americans suffer from both conditions though and according to the End-Stage Renal Disease Incident and Prevalent Quarterly Update, approximately 37% of patients with ESRD have diabetes. (1)
Diet becomes even more important for patients with both conditions. You will need to pay more attention to the amount of carbohydrates (sugars) that you eat. Carbohydrates can be found in many foods such as fruits, milk, breads, deserts and many drinks. Sodium remains important for both CKD and diabetic patients. Keeping your diet lower in sodium helps to lower blood pressure and reduce fluid retention. Protein is another nutrient that has enhanced importance and too much protein can be harmful for diabetic patients. It is important to talk to your dietician and nephrologist to determine the levels appropriate for your care. Another major change from only a kidney friendly diet is emphasis on eating on a routine and balancing out your meals and snacks.
Peritoneal dialysis patients that also are diabetic need to be extra careful with their sugar levels, because dialysate solutions used to clean the body are normally sugar based solutions. Your care team will help determine what solution is best for you and help you adjust your diet to account for the extra sugar in the dialysate. Your care team should be aware of your status as a diabetes patient, however be proactive and make sure your dialysis care team is aware of your condition.
The Following are examples of foods and drinks that are can be exchanged and are good for both diets:
Fruits
-
Good alternatives: Berries, grapes, cherries, apples, plums
-
Avoid: Cantaloupe, mangos, kiwi, oranges, pomegranate
Vegetables
-
Good Alternatives: Cauliflower, onions, asparagus, eggplant, turnips
-
Avoid: Okra, spinach, potatoes, artichokes, tomatoes
High Protein Sources
-
Good Alternatives: Lean meats (poultry, fish), eggs, unsalted seafood
-
Avoid: Bacon, hotdogs, lunch meats, pepperoni, nuts
Drinks (remember your fluid restrictions)
-
Good Alternatives: Water, clear diet sodas, crystal light, unsweetened tea
-
Avoid: Dark sodas, beer, sugary drinks such as Hawaiian Punch or Sunny Delight, Sweet tea or lemonade
Starches
-
Good Alternatives: White bread, bagel, sandwich bun, unsalted crackers, pasta
-
Avoid: Whole wheat or whole grain breads, sugar coated cereal, pancake and biscuit mix, potato chips
Other items to watch out for are condiments such as ketchup or soy sauce and overly sweet items such as candy or cakes. Your health care team may recommend that you follow a meal plan to help manage your dietary needs. A meal plan or a food journal are powerful tools that allow you to track exactly what and when you are eating. Two methods recommended by dieticians are:
- The Exchange Method: A personal meal plan is developed with the help of your renal dietitian. You can make a serving exchange from a list of foods that have about the same nutritional value. Your dietitian or a certified diabetes educator can help you tailor a plan that works for you. An example of this is exchanging out whole wheat bread for white bread to reduce the amount of phosphorous in your meal.
- Carbohydrate Counting: This involves planning meals based on the total number of grams of carbohydrates you eat for that meal. You must be willing to keep track of the foods you eat and the carbohydrates you’ve been allowed. Reading and understanding food labels is very important and can help you manage this process. The more advanced your plan or journal is will make a big difference. If you keep a journal with the foods you eat, amount and how you feel throughout the day, it can help your dietician make even more informed choices and give you the best advice possible.
Putting together a meal plan that meets the needs of both dialysis and diabetes may seem difficult. Remember, your team is here to help you.
- USRDS 2011 Annual Data Report. United States Renal Data System Web site. www.usrds.org/adr.htm [25].
Following a diet as a transplant patient
After you receive a transplant, it is possible that many of the diet restrictions you had during dialysis will disappear. This however, doesn’t mean that proper nutrition is any less important. Also, if you have other conditions like hypertension and diabetes, you will need to continue following those diet restrictions.
Taking immunosuppressants and anti-rejection medications. (1)
To keep your new organ healthy, you will need to take an immunosuppressant drug. Just like the name sounds it suppresses your body’s immune system response to your new organ. Even with careful matching your body won’t recognize the new kidney as its own and will raise your defenses to get rid of it.
The side effects of the medications vary depending on what you are taking. Work with your medical team and dietician to manage the impact they have on you.
In general, some of the drugs can cause side effects such as weight gain, fluid retention, raise blood pressure and cause increased appetite. (2)
Commonly prescribed medications:
- Tacrolimus (prograf)
- Cyclosporine (Neoral, Gengraf)
- Mycophenolate mofetil (Cellcept)
- Mycophenolat acid (Myfortic)
- Sirolimus (Rapamune)
- Steroid (Prednisone) (1)
Example of possible side effects are:
- Steroids like Prednisone can change the body’s ability to use sugar and can cause blood sugars to rise, and in some patients cause fluid retention.
- Cyclosporine medications can cause magnesium levels to drop.
- Other commonly prescribed medications can lower or increase your potassium levels.
What are the main differences from pre to post transplant?
While recovering from surgery, protein will become more important as will total calories. Additional protein will help aid in the healing process and should come from sources such as lean meats, beans and soy products.
Unless you are retaining water, your fluid restrictions are gone. It is important to drink plenty of fluids to support your new kidney. Also, unless instructed differently, you can resume eating foods high in calcium and phosphorus such as dairy and whole grains. The same goes for potassium rich foods such as oranges can be added back into your diet.
Since you are taking immunosuppressants, you will have more of a risk of food-borne infections so avoid raw or undercooked meats or eggs, unpasteurized dairy or raw milk and take extra precautions when handling your food. You will also need to limit herbal medicines and supplements because they could potentially interact with your medications. Many supplements aren’t regulated the same way as prescription medication and this means that your medical team won’t know how they will work with your immunosuppressant.
Maintaining a healthy blood sugar becomes more important, especially if you are taking a steroid based drug.
Items to avoid
- Raw sushi
- Limit buffets and salad bars
- Grapefruit and star fruit or grapefruit juice (interacts with medications)
- Uncooked cookie dough
- Bean sprouts
- Undercooked meats
What is the same as your renal diet?
Certain restrictions remain the same. You should maintain a low sodium diet. Stick to a heart healthy diet including healthy fats to give your new kidney the best chance of survival. Continue to limit grapefruit not for potassium, but because it has been known to increase the immunosuppressive level. (3) Continue to limit your alcohol consumption as it will add extra calories.
Weight gain is common in transplant patients, because of the lack of as many food restrictions, increased appetite and the interaction of medications. It is important that you talk with your medical team to discuss whether this is an issue for you or not. To reduce the amount of weight you gain, avoid high fat and high sugar foods. Also as long as your doctor agrees, you can use exercise to maintain a healthy weight.
It is important to remember that a kidney transplant is not permanent, especially in younger patients. However, following a healthy diet after transplant can help make the organ last longer and improve the quality of your life.
- After Your Kidney Transplant. The Renal Network, Inc. http://www.therenalnetwork.org/services/resources/TransplantBooklet.03.2010.pdf [26]
- Mayo Clinic Staff. Prednisone and Other Corticosteroids: Balance the Risks and Benefits. Mayo Clinic. www.mayoclinic.com/health/steriods/HQ01431 [27]
- Zertasky K. Consumer Health. Mayo Clinic. www.mayoclinic.com/health/food-and-nutrition/AN00413 [28]
Emergency Diet
Emergencies happen every day and the more prepared you are for an emergency the better your outcome will be. Depending on the situation and on the stage of your kidney disease, you may be without your normal clinic or unable to grab all of your home supplies.
You should have an emergency survival kit that includes:
- Food and water for each person for three days
- Flashlight with fresh batteries
- First aid kit
- Three days’ worth of medications
- Prescriptions and instructions to administer in case you are unable to communicate
- Emergency numbers for your doctors and or dialysis center
If you are a dialysis patient, your emergency three day meal plan should have about 40-50 grams of protein, 1500 mg of sodium, 1500 mg of potassium and 16 ounces of fluid for each day. (1) An example set of materials from Davita can be found here.
The following food items will be needed for the 3-day emergency diet and should be stored in your emergency kit (2):
- 3 packages of dry milk or four 8-ounce cans of evaporated milk
- 1 to 2 gallons of distilled or bottled water
- 2 packages of powdered fruit flavored drink or one large bottle of pre-mixed fruit flavored drink
- 1 to 2 cans or bottles of soft drink (no dark cola due to high phosphorus)
- A six pack of 4-ounce cans or boxes of low potassium fruit juice (apple, grape, etc.)
- 6 boxes of single serving cereal (no raisin bran)
- 1 box of sugar, sugar packets or artificial sweetener
- 12 four-ounce cans of low potassium fruit or fruit bowls (peaches, pineapple, oranges, mixed fruit, applesauce or pears. No raisins.)
- 8 small cans of unsalted tuna, salmon, chicken or turkey
- 1 jar of peanut butter
- 1 small jar of grape jelly
- 1 small jar of honey
- 3 small jars of mayonnaise (you will open a new jar each day) or 8-12 single serving foil wrapped packets
- 1 loaf of white bread (this can be stored in the freezer and replaced every 3 months until needed for emergency)
- 1 box of vanilla wafers or graham crackers
- 4 to 6 bags of hard candy (jelly beans, mints, sourballs, lollipops)
- 1 package of marshmallows. (2)
It is important that you don’t panic and missing a dialysis treatment or two is bad, but in all likelihood not life threatening, especially if you follow the further restricted emergency diet.
If you have to evacuate, follow the emergency instructions and immediately alert support personal of your medical conditions.
- Preparing for Emergencies: A Guide for People on Dialysis. Department of Health and Human Services. www.kcerocoalition.com/pdf/101501.pdf [29]
- Emergency Preparedness for People with Kidney Disease. DaVita. http://www.davita.com/kidney-disease/overview/living-with-ckd/emergency-preparedness-for- people-with-kidney-disease/e/4930 [30]
Community support and resources
You don’t have to deal with kidney disease all by yourself. Get support from friends and family. Your family and friends can give you a ride to your treatments or help you grocery shop. They can also offer emotional support when you’re feeling low. Give them a chance to cheer you up or simply listen to you. Support [31]is also available from a variety of sources.
Your health care team offers another level of support. Your doctors, nurses, and renal dietitian can talk to you about your progress, so make the most of the time you spend with them [31]. One way to do that is to ask a family member or your social worker to help make a list of questions [31] for you to ask during your next appointment.
You may find it easier to talk with people you meet at your dialysis clinic or in a support group, if you belong to one. They’ll know what you’re going through and might be able to give you suggestions on sticking with your [31] diet or staying on track with your medications.
Having a community of support is important. You’re less likely to miss medical appointments if you ask for a ride when you need it. Perhaps you’ll eat healthier if someone helps with the cooking or menu planning. And it may be easier to stay on track with your medications [31] with someone to remind you or pick up a prescription for you.
Knowing you have people to rely upon may be a source of comfort and give you peace of mind, too. So reach out for the support you need!
Be ready to talk with your health care team
Before you visit your doctor, have a plan ready. Here are some tips for building a good partnership with your health care provider:
- Before you go, make a list of anything you need to talk about. Are you having new symptoms? Are you having trouble taking your medication? [31] Are you anxious about your treatment? Whatever it is, talk to your health care provider. Many of these issues are fairly common and your health care team can help you work through them.
- Take along any information the doctor or staff may need such as insurance cards, names of your other doctors, or your medical records. Also, bring a list of medications you take.
- Consider bringing a family member or friend. Let him or her know what you want from your visit so you have someone to remind you if you forget.
- Update the doctor. Let your doctor know what’s happened since your last visit, including emergencies or changes in your weight, sleep patterns, appetite, and energy level.
- If your doctor asks about your personal life, this is to see if there are any stresses or changes in your life. Be as honest and open as you can. The more information your doctor has, the better.
- Ask questions! If there’s something you don’t understand, ask. Your doctor is there to help you [31]. If you’re not comfortable speaking up, perhaps a friend or family member can do it for you.
- Take notes. It can be difficult to remember everything you need to remember, so you or your friend should take notes. You may also tape record your visit to play it back later.
- Whenever possible, have the doctor or staff give you written instructions. Ask for brochures, tapes, software, or Web sites that could help you manage your condition.
- Remember that your medical care and health outcome are improved by being an active participant. Y our medical staff can’t treat what they don’t know about.
Other resources
There are organizations you can turn to for more help and information. Here are a few:
Dialysis Patient Citizens (DPC)
1012 14th Street, NW, Suite 905
Washington, DC 20005
Toll-free: 866-877-4242
FAX: 202-789-6935
dpc@dialysispatients.org [32]
American Association of Kidney Patients (AAKP)
3505 E. Frontage Road, Suite 315
Tampa, Florida 33607
800-749-2257
www.aakp.org [33]
American Kidney Fund (AKF)
6110 Executive Blvd., Suite 1010
Rockville, MD 20852
800-638-8299
www.kidneyfund.org [34]
National Kidney Foundation (NKF)
30 E. 33rd St.
New York, NY 10016
800-622-9010
www.kidney.org [35]
National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC)
3 Information Way
Bethesda, MD 20892-3580
800-891-5390
www.kidney.niddk.nih.gov [36]
Renal Kidney Support
For free kidney-friendly cookbooks,
call (866) 896-6152 or
visit www.fosrenol.com [37]
to order your copy today.
Summary
Your diet is an extremely important part of your health and can have a large impact on slowing down the progression of CKD, making your treatments most effective if you require dialysis and will help your transplant last longer.
Work with your healthcare team to fine tune your diet and increase your health and happiness!
Choose Another Class
Congratulations on finishing the class on nutrition management! Please select one of the classes below to continue your educational journey.
Choose Another Class
Congratulations on finishing the class! Please choose another class from the list below to continue your journey.